1 | Overview
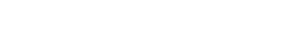
The Planner Guide for K-12 Schools (“The Guide”) is intended to help education leaders and school administrators assess:
Whether current anti-COVID strategies need to be changed in order to decrease the risk of an outbreak.
Whether an asymptomatic screening program is needed, given the anti-COVID strategies you're using.
How frequently asymptomatic screening should happen, given the type(s) of test available.
This Guide is a companion volume to whentotest.org and the WhenToTest Workplace Testing Planner (“The Planner”). The Planner was developed by the Massachusetts Institute of Technology Institute for Data, Systems, and Society and the Massachusetts General Hospital Consortium for Improving Medicine with Information and Technology.
To use the Planner, you will be prompted to enter six inputs, which correspond to the number of people who will be participating in your testing program, the anti-COVID strategies you're using (including vaccination, reliable mask-wearing, close-contact identification and notification, and cohorting participants in unmasked indoor activities), and your district's location. Based on these assumptions, the Planner tells you the following:
Whether you would be able to avoid an outbreak using your current anti-COVID strategies along with an asymptomatic screening program.
How often you would need to conduct asymptomatic screening in order to decrease the risk of an outbreak.
Whether your anti-COVID strategies are strong enough that you no longer require asymptomatic screening and need only test individuals with COVID-19 symptoms.
In addition, the Planner shows how the type of test you use for screening (antigen vs. PCR, individual vs. pooled, on- or off-site) affects the frequency of testing as well as many other details of your testing program, including staffing needs and cost.
Please note that the Planner does not guarantee that COVID-19 will not enter your school, nor does it ensure that all COVID-19 infections will be eliminated. The Planner helps determine the testing frequency needed to identify and isolate potentially contagious people. The rate at which potentially infected people may enter your school is determined by the disease prevalence in the broader community.
The Planner will be updated as new tests are approved and new studies become available. Please return to whentotest.org often.
The WhenToTest Workplace Testing Planner demonstrates how key prevention and containment strategies impact whether and how frequently your school needs to test people without COVID-19 symptoms in order to maintain in-person learning.
BASELINE TESTING
The Planner works best when baseline testing has been performed before starting a screening program. Baseline testing means that 100% of your population is tested and that any individuals who test positive are isolated. It gives you a “clean slate” in which any COVID-19 infections that arise come from outside the school.
If you’re planning to start an asymptomatic screening program, then one complete screening cycle in which everyone participates will address this need. If you are unable to test 100% of your population either as a baseline or during asymptomatic screening, don’t worry — you can still use the Planner. However, if the disease prevalence is very high in your area, you’ll need to be much more careful about your other anti-COVID strategies. For more details, see Additional Guidance for Using the Planner.
Fire Analogy for Mitigating COVID‑19
To Prevent a Fire
Unplug/limit use of electric toaster ovens
Limit use of electric heaters
Get a permit for open outdoor fires
Fire prevention does not guarantee a fire will never happen. The same is true for COVID-19. Key precautions are simple, affordable, and smart behaviors to maintain safety.
To Prevent COVID‑19
Support vaccination
Wear masks
Improve ventilation
To Contain a Fire
Activate sprinkler systems
Sound alarms and alert 911
Evacuate the building
If a fire or virus outbreak does happen despite taking precautions, then containment strategies limit the loss of property and lives.
To Contain COVID‑19
Notify close contacts quickly
Isolate and quarantine
To Detect a Fire
Maintain smoke alarms
Install carbon monoxide detectors
Use thermal imaging cameras
Warning systems can’t prevent fires nor can diagnostic tests prevent COVID. They are alarms that set containment strategies into motion.
To Detect COVID‑19
Screen asymptomatic people
Test symptomatic people
2 | Inputs
Just as fire-prevention methods do not guarantee a fire will never happen, there is no guarantee that COVID-19 will not enter your school. However, several simple, affordable, and smart strategies have proven to significantly decrease the spread of the virus.
To start using the Planner, enter the number of people who will be participating in your testing program, the anti-COVID strategies you're currently using, and the location of your school district. As you continue to work with the Planner, you can see how adjusting your anti-COVID strategies affects your testing needs.
PEOPLE BEING TESTED
What percentage of your total population will participate in your COVID-19 testing program?
When you first use the Planner, enter the total number of people – faculty, staff, and students – in school on a normal day and the percentage of people who will participate in your COVID-19 testing program. Later, you may want to model groups of people within your school whose anti-COVID strategies are somewhat different from one another, to see how their testing needs might differ. For example, consider an elementary school in which the vaccination rate is 75% for teachers but only 50% for students. When you model the teachers and students separately, the Planner will recommend very different testing frequencies for each group.
VACCINATION
What percentage of people in your school have been fully vaccinated? Have most people in your organization received booster shots?
Your number-one weapon against COVID-19 is vaccination. Increasing vaccination rates in your school population will do more to reduce your testing needs than anything else. Fully vaccinated = having received two doses of an mRNA vaccine (Pfizer or Moderna) or one dose of the Johnson & Johnson vaccine. In some states, the department of public health can arrange on-site vaccination clinics at schools or field trips to vaccination sites. Many private schools require vaccines for all faculty, staff, and students; for public schools, vaccine requirements are typically set by the state.
USING THE PLANNER
If you do not know the percentage of people in your school who have been vaccinated and boosted, use the published rates from your county.
If you plan to test only the unvaccinated members of your population, then the number you input for this question should be 0.
MASKING
What percentage of people reliably wear masks while at school? What kind of mask do most people wear?
Masks offer protection to the wearer and also protect others if the wearer is infected with the virus that causes COVID-19. A well-fitted mask, worn properly, covers both the nose and mouth and fits snugly against the sides of the face, without leaving gaps. The CDC also recommends wearing masks with nose wires, to prevent gaps in that area. Consistent indoor mask-wearing among your school population will greatly reduce your testing needs and, therefore, reduce your costs.
The type of mask people wear matters. Two-layer cloth masks have a filtration efficiency of about 30%. For surgical masks that fit well, without gaps, that number is about 70%. For KN95 masks, it’s about 85%.
USING THE PLANNER
In the Planner, the input “What percentage of people reliably wear masks?” refers to the estimated percentage of students, faculty, and staff who wear masks appropriately at all times when indoors within your school. It is common to overestimate reliable mask usage, so using a lower percentage than you initially selected may give you a more accurate result. For example, if your school requires masking at all times when indoors, consider modeling with the Planner input for masking at 75%.
If your school no longer has a mask policy, input “0” in this section of the Planner.
IDENTIFYING AND NOTIFYING CLOSE CONTACTS
Can your organization identify and notify close contacts within 24 hours? The goal of contact tracing is to identify the people who were in close contact with an infected person while they were contagious, so that those people can be prevented from spreading the disease to others. The faster close contacts are identified and notified of their status, the sooner they can quarantine or be enrolled in your school’s test-to-stay program, and the less likely it is that they will infect other people. If you can identify and notify close contacts within 24 hours, your need for testing will decrease.
In practice, identifying exactly who has been in “close contact” with someone can be quite difficult unless your school keeps good records. Seating charts can be very helpful for this purpose; teachers may also want to keep track of which students tend to walk together in the hallways. If you’re not sure what percentage of close contacts in your school are identified and notified within 24 hours, check with the school nurse or other staff member in charge of this task.
USING THE PLANNER
The Planner assumes that only 50% of close contacts are identified and notified, but many schools are able to do better than that. If you know your school’s efficiency in this area is above or below 50% (0.5), go to the Results page and click on Show Advanced Settings (see yellow arrow).
Then click on Main Planner Settings (green arrow), find Contact Identification Efficiency (red arrow), and adjust the default there.
COHORTING WHEN UNMASKED
Do individuals in your organization ever gather indoors in close proximity (for example, while eating) without wearing masks? Does anyone in your organization participate in high-COVID-risk activities such as sports, singing, or playing wind instruments while unmasked? (High-COVID-risk activities are those in which people breathe heavily or with force.)
When people are indoors and unmasked, some activities carry higher risk of virus transmission than average day-to-day interactions. These activities involve either gathering close together for extended periods of time (most commonly while eating or drinking) or breathing heavily and/or with force.
To decrease the risk of COVID-19 in these situations, keep the cohorts of people who participate in them as small as possible. In the example below, two cohorts of four students eating lunch are separated by six feet of distance. Other examples of unmasked cohorts would be a basketball team, a choir, or a marching band, if those groups participate in their activities indoors and unmasked.
USING THE PLANNER
If people participate in high-COVID-risk activities indoors and unmasked at your school, enter the size of the largest cohort of people who either gather in close proximity or who participate in another high-COVID-risk activity together. For example, if there are 10 people in your choir and 20 on the basketball team, enter “20.” If lunch is the only time when people are allowed to be unmasked together, enter the size of the largest group of people who eat lunch at the same table.
If unmasked indoor group activities are not permitted, or if people eat lunch indoors alone and no other indoor unmasked activity is permitted, input “0.”
Often, people neglect to account for eating activities or smoke breaks as unmasked indoor activities. Remember, chatting for 10 minutes with your mask at your neck while getting coffee is considered an unmasked indoor activity.
LOCATION
What county is your organization in?
The Planner makes its recommendations based on how many people carry the virus in your area, which is estimated at the county level. If your school is in a US territory (other than Puerto Rico) or outside the US, you will need to tell the Planner whether you are in a hotspot or not. For the purposes of the Planner, your area is in a hotspot if there have been at least 100 cases of COVID-19 per 100,000 people in your area over the past seven days, and/or the test positivity rate in your area is currently 10% or higher.
ADDITIONAL MITIGATION MEASURES
IMPROVED VENTILATION
The virus that causes COVID-19 can be transmitted by aerosols: microscopic droplets of liquid that can float in the air. Improving ventilation is a critical anti-COVID strategy because it helps to reduce the amount of virus-carrying aerosols indoors. Outdoors, aerosols disperse very quickly. That’s why COVID-19 is so rarely transmitted during outdoor contact.
Methods that improve indoor ventilation and air cleanliness include:
Opening windows and doors (if consistent with school safety protocols).
Placing a fan safely and securely in a window to pull room air outdoors.
Reducing or eliminating heating, ventilation, and air conditioning (HVAC) air recirculation, and implementing ventilation system upgrades or improvements (all in consultation with experienced HVAC professionals).
Using portable high-efficiency particulate air (HEPA) filtration systems, especially in more confined or higher-risk areas such as nurse’s offices (these work best when positioned at head height).
Installing ultraviolet germicidal irradiation (UVGI) units in HVAC systems or at ceiling level (if ceiling height permits).
Portable carbon dioxide (CO2) monitors can be used to check the level of ventilation in a room. If the CO2 level is above 800 parts per million (ppm) during normal occupancy, then the ventilation needs to be improved. If increased ventilation does not bring the levels down enough, then HEPA filters and/or UVGI units are necessary.
DISTANCING To whatever extent is possible, unvaccinated individuals should remain physically distanced when indoors. Ideally, unvaccinated students should be spaced at least three feet apart from one another and six feet apart from teachers when in the classroom. Unvaccinated teachers should also remain six feet apart from one another if possible. HAND HYGIENE Teach and reinforce handwashing with soap and water for at least 20 seconds and increase monitoring to ensure adherence among students and staff. Hand sanitizer that contains at least 60% alcohol should also be made available. Clean frequently touched surfaces within the school and on school buses daily.
3 | Outputs: Testing Strategies
Once you have entered the inputs, the Planner will recommend a range of testing strategies based on how strong your anti-COVID strategies are.
Just like a smoke alarm is a detection strategy for a fire, testing is a detection system for a potential COVID-19 outbreak. Testing to detect COVID-19 is part of a comprehensive strategy and should be used along with other behaviors that reduce spread.
Because there is no one-size-fits-all plan, schools should determine, in collaboration with local health officials, whether to have a testing program and if so, how best to manage it. For many schools, testing will be a critical aspect of their pandemic resilience plan.
The WhenToTest Workplace Testing Planner is designed to support this decision making, helping you determine:
Whether asymptomatic screening is right for your school or if only symptomatic testing is needed.
Frequency of asymptomatic screening based on several different test methods.
Costs for each testing scenario.
Ultimately, the type of test used in your school will be decided based on test availability, cost, and timeliness of results. In many cases, a single test or a range of test vendors will be selected at the state level. No matter what test is chosen, it is essential for school decision-makers to understand the strengths and weaknesses of that test and how best to assess and act on test results.
In addition to state and local laws, school administrators should follow guidance from the Equal Employment Opportunity Commission when offering testing to faculty, staff, and students who are employed by the school. Schools should also follow guidance from the US Department of Education on the Family and Educational Rights and Privacy Act (FERPA) and the Health Insurance Portability and Accountability Act (HIPAA).
IMPORTANT INFORMATION
The Planner provides results for several types of COVID-19 test. The test types are examples; none of them represent any one individual test. The performance and cost of individual tests can vary significantly, even if they are the same general type of test.
The sensitivity and specificity chosen for each test type is a conservative estimate for asymptomatic screening based on consultation with industry experts.
The Planner provides guidance for asymptomatic screening of an organization under health-care practitioner guidance. This type of screening is off-label use for most tests.
Test results should be received and reviewed within 24 hours (one day) of sample collection so that contact tracing is as effective as possible.
COVID-19 cases must be reported, by health-care providers and laboratories, to state, tribal, local, and territorial (STLT) health departments. All case investigation and contact tracing support activities in your school should be undertaken in coordination and agreement with your local department of public health.
School-based testing should NEVER be conducted without consent from a parent or legal guardian (for minors) or from the individual themselves (for adults).
Navigating the Results Page
The results page of the Planner has four main sections.
The Input Bar allows you to change the inputs so that you can see how changing your anti-COVID strategies affects your testing needs.
The Results Tables show you the Planner’s recommended testing strategies based on your inputs. When you first see this page, the table on the left will provide your first-pass results. (If you skipped the Guided Entry, a default scenario will appear on the left.)
When you make changes to the inputs, a new set of results based on those inputs will appear on the right.
At the top of the page you can save the scenario in the right column under a new name.
Asymptomatic Screening or Symptomatic Only?
If your anti-COVID measures are very strong, the Planner will recommend symptomatic screening only: testing only people who show symptoms of COVID-19 (see green box below).
In many cases, the Planner will show that you can help reduce the risk of an outbreak by adding asymptomatic screening to your mitigation strategies (see yellow box below). Asymptomatic screening is intended to identify infected people who do not have known, suspected, or reported exposure to SARS-CoV-2 (the virus that causes COVID-19), and who also have no symptoms of the disease. A variety of types of COVID tests can be used for screening. Because those tests have different characteristics, the Planner provides different recommendations as to how frequently testing should take place. We will cover the differences between the various test types in the Types of Tests section.
In some situations, the Planner will return a result that indicates an outbreak is likely (see red box below). If that happens, consider how your school might strengthen anti-COVID measures other than testing: by improving access to vaccination and boosters, emphasizing consistent mask-wearing and use of higher-quality masks, keeping better track of close contacts, or decreasing the size of cohorts that participate in unmasked activity together.
Types of Tests
The Planner provides recommendations based on several different test types. The test types differ from one another in three main ways: the type of chemistry they use, where the samples are analyzed, and how many people’s samples are tested at one time. CHEMISTRY: ANTIGEN VS. PCR Antigen tests (see red boxes below) detect proteins from the virus. They tend to be quick (results in under an hour) and less expensive than lab-based PCR tests, but because they aren’t as sensitive as PCR, they can misdiagnose infected people who are carrying very small amounts of virus. They also aren’t as specific as PCR, so they may require confirmatory tests.
PCR tests (see blue boxes below), also called molecular tests, detect genetic material from the virus using a lab technique called polymerase chain reaction (PCR). PCR test can detect very small amounts of virus, so they can diagnose an infection very early. Results should take no longer than 24 hours (one day) to arrive from commercial labs; on-site PCR tests take under an hour.
ANALYSIS LOCATION: ON-SITE VS. OFF-SITE
On-Site Testing: Also called point-of-care (POC) testing. Samples are collected and tests are run at the school. These tests provide same-day results, but most require trained staff to run them, and most also require that the school be certified under the Clinical Laboratory Improvements Amendments (CLIA). (See red boxes below.)
Many point-of-care tests are now available over the counter (OTC). Also called home-based tests, they can be done anywhere, and the samples can be collected and analyzed by the individuals being tested. However, reporting of results for these tests may need to be done on the honor system.
On-site tests on a small instrument: Most schools will require multiple instruments in order to test enough people quickly. In addition, the instruments require trained staff to run and maintain them.
Off-Site Testing: Also called lab-based testing. Samples are collected at the school and sent to a commercial laboratory for analysis. Select a lab that can provide results within 24 hours (one day) after samples are collected. (See blue boxes below.)
SAMPLES PER TEST: INDIVIDUAL VS. POOLED
The first four test types that the Planner displays in the Results Tables are individual tests. The fifth row in the tables is a pooled test (see red box below) If you click on View More Pooling Options below the tables, you can see recommendations for additional types of pooled tests.
How follow-up testing is done depends in part on where the pooling takes place.
In-lab pooling (see red boxes below): Individual swabs or vials of saliva go to the lab and are pooled there. The lab saves each individual sample so that when a pool tests positive, all individuals in that pool can be tested automatically.
On-site pooling (see blue boxes below): Individual swabs are placed into the same test tube at the school before being sent to the lab. When the lab finds a positive pool, all members of the pool must be re-swabbed and individually tested.
The Planner identifies four strategies for follow-up testing of a positive pool. The strategy you choose will depend on a variety of factors, including recommendations or requirements from your state department of education, the logistical constraints of your school or district, and the personnel required for testing and sample acquisition. Funding for COVID-19 testing in public K-12 schools is currently being provided by the federal government. For private schools, the cost of testing will also factor into your choice of testing strategy.
The table below reviews how the four follow-up strategies work and what their strengths and weaknesses are.
FOLLOW-UP STRATEGIES FOR POOLED TESTING: PROS AND CONS
Follow-Up Test Type | Pooling Process | Follow-Up Testing Process | Pros | Cons |
|---|---|---|---|---|
Automatic | Individual samples collected on-site and shipped to off-site lab. Lab creates pools and tests pooled samples using PCR. | Lab keeps original samples and retests them individually with PCR. | Eliminates need to re-collect individual samples. Results provided faster than other pooled testing strategies. | May be 2-3x more costly per test than rapid antigen and on-site PCR follow-up. |
On-Site Rapid Antigen | Individual samples collected and pooled on-site. Pooled samples are shipped to off-site lab for testing using PCR. | On-site staff re-swabs and retests individuals with rapid antigen tests. | Faster than off-site PCR follow-up. Likely to be least expensive option. | Requires re-swabbing individuals in positive pool. Requires trained staff on site. Slightly less accurate than PCR follow-up. |
On-Site PCR | Individual samples collected and pooled on-site. Pooled samples are shipped to off-site lab for testing using PCR. | On-site staff re-swabs and retests individuals using PCR instruments. | Faster than off-site PCR follow-up. Less expensive than automatic or off-site PCR follow-up. Highly accurate. | Requires re-swabbing individuals in positive pool. Requires trained staff on site. Requires purchase and maintenance of instruments. |
Off-Site PCR | Individual samples collected and pooled on-site. Pooled samples are shipped to off-site lab for testing using PCR. | On-site staff re-swabs individuals; samples sent to off-site lab for PCR tests. | Highly accurate. | Requires re-swabbing individuals in positive pool. Slowest pooling option. More expensive than on-site follow-up. |
Test Type Overview
Just as no fire-sensing device is perfect, no test is perfect — they all have trade-offs.
Smoke Detectors
Early warning
False alarms happen
Good at true negatives (no fire)
Off-Site PCR Tests
Detects disease even without symptoms
Slower turnaround
Good at confirming that someone doesn't have disease
Thermal Imaging Cameras
Real-time results
Not good for early warnings
Better at true positives (TOO HOT)
Point-Of-Care Antigen Tests
Inexpensive
Same-day results
Can miss infected people who don't have symptoms
If you have a choice of what kind of test to use, the WhenToTest Workplace Testing Planner can help you make an informed selection. If your state has mandated a specific test type, the Planner can help you determine how frequently you need to test, evaluate whether you need to adjust your anti-COVID strategies, and assess test results and respond to them appropriately. The table below shows the strengths and weaknesses of the five major test types covered in the Planner: Rapid antigen, on site; antigen with instrument, on site; PCR, on site; PCR, off site; and pooled PCR.
Major Test Types — Strengths and Weaknesses
Test Type | Strengths | Weaknesses |
|---|---|---|
Rapid Antigen, On Site | Typically lowest cost. Fast turnaround time. | May give false negative results in people without symptoms or false positive results in low-prevalence environments. Typically requires more frequent testing than PCR. May require CLIA waiver and trained staff. Can’t conduct many tests at once. |
Antigen with Instrument, On Site | Fast turnaround time. | May give false negative results in people without symptoms or false positive results in low-prevalence environments. Typically requires more frequent testing than PCR. May require CLIA waiver. Requires trained staff Instrument(s) must be purchased and maintained. Can’t conduct many tests at once. |
PCR, On Site | Fast turnaround time. More likely to detect asymptomatic infection than antigen tests. | Requires CLIA waiver. Requires trained staff. Instrument(s) must be purchased and maintained. Can’t conduct many tests at once. |
PCR, Off Site | Detects nearly all infections – almost no false negatives. Can test a lot of people at once. | Most expensive option. Slower turnaround time. |
Pooled PCR | Lower cost than individual off-site PCR. Detects nearly all infections – almost no false negatives. Best at testing a lot of people at once. | More expensive than on-site options. Pooling strategies that require re-swabbing have slowest turnaround time. May need CLIA waiver and/or trained staff, depending on follow-up strategy. |
Test Frequency
Along with your other mitigation measures, the Planner takes the strengths and weaknesses of the tests into account. Because of the differences between the tests, how often your school needs to test may vary depending on the type of test you use. For example, in the scenario on the right, in order to decrease the risk of an outbreak using an on-site rapid antigen test without an instrument, you would need to test your population once a week (see red box below). Using an antigen test with instrument, you would only need to test every other week (see blue box below).
Comparing and Saving Scenarios
The two tables at the bottom of the screen are designed to allow you to see how changing your organization’s mitigation strategies will change your testing needs. You can also use the tables to compare groups of people within your organization who have different mitigation strategies and/or different environmental conditions. The first time you see the results page, the table on the left will provide your first-pass results. (If you skipped the Guided Entry, a default scenario will appear on the left.) The scenario on the left will not change when it is in that position.
When you make changes to the inputs, a new set of results based on those inputs will appear on the right. The scenario that appears in the right-hand column is intended to be used for comparison with the scenario on the left.
Once you’ve created and saved new scenarios, you can use the dropdown menus above the tables to choose which scenario you want to display in each column (see green boxes below). You can edit any scenario by placing it in the right-hand column and changing the inputs at the top of the page.
4 | Communicating Your Strategy and Results
Open communication with your larger school community about your COVID-19 strategy can help reduce anxiety regarding participation in testing and contact tracing and help build trust in the process, which will be critical for its success. Be sure to listen to and address the concerns of teachers, staff, students, families, caregivers, and guardians.
We recommend holding (virtual) school- and community-wide communications events to:
Communicate school policy regarding COVID-19 precautions.
Demonstrate the Planner and show how decisions on testing type and/or frequency were made.
Provide information about the tests (and the lab that will be processing them, if applicable).
Describe the logistics of the testing program, including how long testing will take for students and educators, how individual privacy will be maintained, and how parents and guardians can provide consent for testing.
Ensure that school employees have a specific point of contact for accessing health and safety support.
Ensure that families, guardians, and school employees have a specific point of contact for accessing testing program support.
Getting buy-in from teachers and from students themselves is often the key to creating a successful testing program.
As part of planning a testing program, your COVID team will need to determine how data will be collected and how that data will be shared with the community. Not only will you want to know whether your COVID-19 precautions were able to prevent outbreaks, but you should also be able to use the data to make informed decisions about whether and how those precautions need to change over time.
Many schools use an online dashboard to communicate testing results to the community. Dashboards are most useful when they clearly describe what anti-COVID measures are in place, including policies regarding isolation, quarantine, and your district’s test to stay program (if applicable). Transparent communication on these topics will help promote confidence both in the testing process and in the safety of in-person learning. A sample dashboard appears below.
Student Data
Current COVID-19 confirmed positive
0.2%
12 students
Current percentage of students quarantined
3.2%
232 students
Total COVID-19 positive cases
95
Since October 21, 2020
What to do if you test positive
Per CDC guidelines, you must isolate for at least 5 days.
You can stop isolating after 5 days if you don’t have a fever and your other symptoms are getting better. Wear a mask around others for the next 5 days, and don’t travel. If you can’t wear a mask, keep isolating for that second group of 5 days.
If your immune system doesn’t work properly, check with your health-care provider before ending isolation.
It’s a good idea to get tested after the first 5 days are over, because you may still be contagious. If you test positive, you should continue to isolate and test yourself again in a day or two. You may end up needing to isolate for 10 days.
What to do if you are a close contact
What you’ll need to do depends on whether you’re vaccinated or not. Please contact the school nurse for instructions.
DO YOUR PART - STAY UP TO DATE ON YOUR VACCINATIONS!
5 | Additional Guidance for Using the Planner
While the Planner provides results for a variety of different test types, remember that the test you have access to is always your “best test.”
If the Planner’s recommendations for the type of test you have aren’t feasible, or if they indicate that you cannot prevent an outbreak using that type of test, consider how you can improve other anti-COVID measures at your school. Use the Planner to model various scenarios and predict how improvements in vaccination, mask-wearing, close-contact identification, and decreasing the size of unmasked cohorts can change your test recommendations.
The Planner works best when you have performed baseline testing (testing 100% of your population and isolating any individuals who test positive) before starting an asymptomatic screening program. However, in many schools, that simply isn’t possible. If the prevalence of COVID-19 is low in your surrounding community, the Planner’s recommendations are likely to be the same with or without baseline testing, and no additional action is needed. However, if your school is in a geographic area with a high COVID-19 prevalence, you will need to be particularly vigilant about your mitigation measures other than testing in order to decrease the risk of an outbreak.
The virus has continued to mutate over the course of the pandemic, giving rise to what are called variants.(A variant is a mutated form of the original or “wild type” virus.) When more-transmissible variants become highly prevalent in your geographic area, your testing needs may change, as well. We recommend that you recheck your testing needs with the Planner periodically, to make sure that your testing program stays up to date.
6 | Resources
The WhenToTest Workplace Testing Planner brings the latest testing strategies into a single innovative modeling tool that demonstrates how vaccinations, masking, contact tracing, limiting unmasked group activities, and screening for COVID-19 can decrease the likelihood of an outbreak at your school. Many additional considerations will factor into your COVID mitigation plans. We recommend reviewing the CDC and OSHA guidelines on the following topics to further aid in your decision making and planning:
Additional Resources:
CDC and Shah Family Foundation - Open and Safe Schools A web-based toolkit for planning and implementing a school’s COVID-19 screening program.
Chiefs for Change - Project Planning Workbook for K-12 COVID-19 Testing A spreadsheet-based checklist for planning and implementing a school’s COVID-19 screening program.
SalivaDirect - Every School Safe and Open A comprehensive guide to COVID-19 mitigation in K-12 schools, including downloadable materials in multiple languages and links to all available federal funding sources.
Epidemiology and Laboratory Capacity (ELC) Reopening Schools This money is earmarked specifically to support COVID-19 testing programs in K-12 schools and is flowing through the departments of public health in the US states, territories, and five of the largest cities (New York, Chicago, Los Angeles, Houston, and Philadelphia). For information on how your school can access this funding, contact your state, territorial, or city department of public health.
Elementary and Secondary School Emergency Relief (ESSER) The US Department of Education awarded a series of these grants to the state educational agencies in 2020 and 2021. For more information on ESSER funds, contact your state department of education.
Rockefeller Foundation - K12 National Testing Action Program
CMS - Over The Counter (OTC) Home Testing and CLIA Applicability
7 | About Us
CORE
CORE is a Los Angeles-based NGO committed to providing immediate and effective community-based disaster relief to the most vulnerable of our community. The mission of CORE is to not only react to disaster but proactively support the communities in the wake of disaster through education, infrastructure projects, neighborhood planning, women’s entrepreneurship and community health programs. Today, CORE is responding to the global pandemic by lending its experience and expertise to providing the necessary testing and social services to those communities that are most vulnerable to devastating effects of COVID-19.
GHC3
The Global Health Crisis Coordination Center was established in March 2020 as a division of the Center for Global Health Innovation by a group of public health and business leaders in Atlanta focused on supporting the private sector public health response to the COVID-19 pandemic, GHC3 was tasked by the CDC Foundation to share information and coordinate resources between public health, private sectors and philanthropic organizations during this global health crisis.
Since its inception, GHC3 has worked closely with corporate partners and the CDC to identify gaps in guidance and formulate best practices for a safe return to school, work and worship in the face of COVID-19. It has stood up over ten strike teams to address issues such as critical equipment needs, equitable distribution of vaccines, and mental health. Its near-term projects include the development of a global health data management system, a collaboration portal to effectively connect resources by leveraging AI, and a health monitoring system for at-risk healthcare workers.
NIH RADx®
The National Institutes of Health launched the Rapid Acceleration of Diagnostics (RADx®) Initiative to speed innovation in the development, commercialization and implementation of technologies for COVID-19 testing. This project has been funded in part through the NIH RADx® Initiative via federal funds from the National Institute of Biomedical Imaging and Bioengineering, National Institutes of Health, and Department of Health and Human Services via NIH grant number U54EB015408. The WhenToTest Workplace Testing Planner was developed by CIMIT at MGH and MIT IDSS with funding from the NIH RADx® Initiative.