COVID and Flu Risk Quiz FAQs
Tests & Testing
Every household in the US can order four free rapid tests at covidtests.gov or by calling 1-800-232-0233 (TTY 1-888-720-7489).
You can purchase over-the-counter at-home COVID tests at many pharmacies and other retail outlets, as well as online. Check with your insurance provider for their reimbursement policy. The Rockefeller Foundation is also offering free at-home COVID tests to individuals in certain ZIP codes through their Project ACT program while supplies last.
If you have COVID symptoms and you don't have health insurance, you can get tested for free through the CDC ICATT program. Find a free testing site here. If you test positive, you may be able to get treatment during the same visit through the Test to Treat program.
You can also contact your health-care provider, your local community health center, or your state or local public health department for more information.
Whenever you test yourself with an at-home test, remember to report your result — whether it's positive or negative.
The COVID and Flu Risk Quiz is a tool intended to help you decide whether you should get tested for COVID or influenza (flu) in order to keep from spreading these diseases to other people. If you get this recommendation, your risk of spreading the disease will be lowest if you get tested before coming into close contact with anyone outside your household. (This Quiz is a decision-support tool only. Results are provided for informational purposes and should not be construed as medical advice.)
There are two basic kinds of test for viruses: molecular tests and antigen tests.
Molecular tests look for pieces of the virus’s genetic material.
The most common type of molecular test is a PCR (polymerase chain reaction) test. That's the kind of test most labs use.
PCR tests are really good at finding very small amounts of the virus - that's called being a very sensitive test.
PCR tests can diagnose COVID very early. But they will also continue to give positive results even when an infection is over, because they're triggered by dead pieces of virus.
Another common type of molecular test is a LAMP (Loop-mediated isothermal AMPlification) test.
Both LAMP- and PCR-based home tests are available. If your test runs on a small machine, it's probably a LAMP or PCR test.
Antigen tests look for proteins from the virus.
Most home tests are antigen tests. If your test looks like the one in the picture below, it's probably an antigen test.
These tests are very good at diagnosing people who are carrying a lot of virus. They are not as good as molecular tests are at finding people who aren't carrying as much virus.
Another type of COVID test you may have heard of is an antibody test, also known as a serology test. It can't diagnose a current COVID infection, but it can tell you whether you've been infected or vaccinated in the past.
Disease Prevention
All available COVID vaccines are very good at keeping people from going to the hospital or dying from the virus. People who are up to date on their vaccines have the least risk of getting very sick. They are also less likely to get infected at all, especially if they received a vaccine recently.
Being vaccinated usually makes you 40 - 60% less likely to get the flu. For the 2023 - 2024 flu season, early research suggests that being vaccinated cuts your risk of getting the flu in half.
CDC — Stay up to Date with Your COVID Vaccines
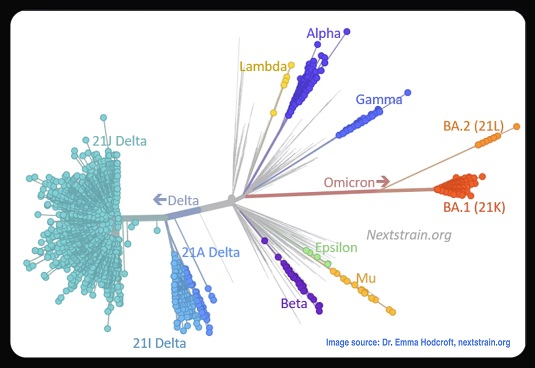
Yes. The Quiz uses an estimate of how well the vaccines available in the US protect against the variant that is currently dominant in the country. This estimate is based on the performance of all available vaccines, not on any one vaccine brand or type.
CDC – Monitoring COVID Vaccine Effectiveness
It depends on the type of mask you wear.
Because Omicron and its daughters are so easy to catch, wearing a cloth mask alone isn't going to help very much. Even a well-fitted surgical mask isn't great. Your best bet is to wear a KN95 or N95. However, when COVID levels are high, wearing any kind of mask is better than not wearing one at all.
Here is what the Quiz assumes about how well the different kinds of masks work:
N95 / KN95: Filters out 85% of particles
Surgical mask: Filters out 70% of particles (Note: This assumes a good fit, with no gaps)
Cloth mask: Filters out 40% of particles
These numbers are based on research that tested how well masks work:
It used to be that if you got infected, your risk of getting infected again was a lot lower for a while — usually about three months. Then the Omicron variant arrived. Now, some people can get COVID again within a few weeks, but it's not clear how common that is.
For those reasons, the COVID and Flu Risk Quiz assumes that if you got infected within the last 45 days, you have a small amount of protection from getting infected right now.
If you've already had the flu this season, it's extremely unlikely that you'll get it again this season. The Quiz assumes that your risk for this season is near zero.
When it comes to getting sick from COVID or flu, some places are riskier than others. How risky a place is depends on two things:
How many infected people are in the space
How much clean air is in the space
Why is that?
COVID moves through the air like smoke. When a room has more fresh air moving through it, you breathe in fewer virus particles. This animation from the University of Oxford shows how COVID moves through the air. (Animation by Vicki Martin, University of Oxford)
That’s why it's riskier to spend time in places that don't have as much fresh air, like bars or cramped stores.
Places where people shout or breathe hard, like nightclubs or gyms, add risk, as well.
The more time you spend in places with infected people, the more likely you are to get infected, too.
Why is that?
We know now that COVID can travel a lot farther than 6 feet, especially indoors. That may be true of flu, too.
We also know it can stay in the air for a long time, especially in places without a lot of fresh air. This animation from the University of Oxford shows how COVID travels in the air. (Animation by Vicki Martin, University of Oxford)
So the longer you spend in a room with a person who has COVID or flu, the more likely you are to breathe in enough virus to make you sick.
Using the Quiz
The Overview
The COVID and Flu Risk Quiz takes information about COVID and influenza (flu) and combines that with information about your activities and your personal history. It then gives you an estimate of how likely it is that you might have either of those diseases right now.
The Nitty-Gritty
The Risk Quiz uses three basic kinds of information:
Data about COVID: This includes estimates of COVID levels around the country based on wastewater data; research on how contagious the latest variant is, and how well vaccines work against it.
Data about flu: This includes CDC reports on levels of flu around the country, the latest information on how contagious this season's strain of flu is, and how well this year's vaccine works against it.
Your history: This includes whether you’ve had either of these diseases recently, whether you're vaccinated, the kind of mask you generally wear, whether you have symptoms right now, and any known recent exposure to these viruses.
Your behavior: This includes the kinds of places you go during a typical week, how clean the air tends to be in those places, and how often you go there; your mask-wearing habits; and any special events you attended last week or plan to attend in the near future.
The mathematical model behind the Quiz uses CDC data about flu and wastewater data about COVID to figure out how likely it is that someone you meet in your area is infected with one or both of those diseases. It converts that information into an estimate: If you were exposed to someone in your area, how likely is it that you would get COVID or flu?
Next, the model looks at your history to see how well-protected you are against infection right now. The better-protected you are, the less likely it is that any one exposure will make you sick.
Finally, the model converts your activities into an equivalent number of exposures. Riskier activities are like being exposed to a lot of people. Less-risky activities are like being exposed to a smaller number of people.
The model then puts all the information together:
How many exposure equivalents you’ve had over the past seven days.
How likely it is that any of those exposure equivalents would infect you.
How well-protected you are.
The result is an estimate of how likely it is that you have COVID and/or flu right now.
Yes.
Most people find out they have COVID by using rapid tests at home. If they don't report their results, the case never gets reported to the CDC. Since that happens a lot, COVID case numbers around the country are often a lot higher than the the CDC's maps say they are. (The CDC knows about this problem, and the government is working on ways to solve it.) The Risk Quiz deals with this issue by using wastewater data. If someone is infected with COVID, they shed virus particles in their waste. Labs can test sewer water to see how much virus people in the area are shedding. We use that information to estimate COVID levels around the country.
Our methods are based on the following research, as well as research done by NIH consultants.
Articles
WhenToTest — For COVID and Flu
At-home combination COVID and flu tests are almost here. WhenToTest is ready to help you use them.
Don’t Feel Like Getting Sick This Winter? Here’s One Weird Trick
There’s this cool thing that can really help keep you from getting the flu, a cold, or even COVID! It’s called a mask.
Reading Roundup: Respiratory Virus Season
Here are our picks for the articles and status updates that will keep you informed this fall and winter.
Going Back to the Office — For Real This Time
How my partner tries to dodge COVID now that she’s been forced back in.
Keep Kids in School by Keeping the Air Clean
Use these tips and tools to help keep kids learning this fall and winter.
Accessible Tests and Why You Should Care
Many design improvements that could make COVID tests more accessible for people with disabilities will make them easier to use for all of us.
Time to Get the Flu Vaccine
The flu season may come early again this year. The time to protect yourself is now.
We're Still Not Done With COVID...Here's Why!
Even though the virus is under control to some degree, there is still a lot of important work happening to understand and improve how we manage it.
EUAs: The Beginning and The End
Emergency Use Authorizations (EUAs) gave us COVID tests quickly. What happens to them when the emergency is over?