Long COVID: The Long and the Short of It
How much do you know about this really unusual condition that has plagued more than 15% of us?
I try to be a good friend. When someone I know has COVID, I check in on them. How are they feeling? Do they need anything delivered? Are they going stir crazy? Testing negative yet? After a week or so, I assume they’re well again. I never think to ask whether they fully recovered. The answer might be “no” in more cases than we realize.
Long COVID is defined as symptoms someone didn’t have before their COVID infection that continue for at least three months after they first got the virus. The ongoing Household Pulse Survey recently reported that 5.8% of adults in the US today are plagued with Long COVID symptoms. That’s more than 15 million people.
Who’s Most Likely to Get Long COVID
While the risk of developing Long COVID is highest for those with severe cases requiring hospitalization, it’s definitely not limited to that group.
More than 15% of people with COVID have also experienced Long COVID, and it’s expected that 90% of people living with Long COVID initially experienced only a mild case of the disease.
Studies have also found that the risk for adult women is twice as high as for men. And despite a lower risk, children are affected too.
What Long COVID Looks Like
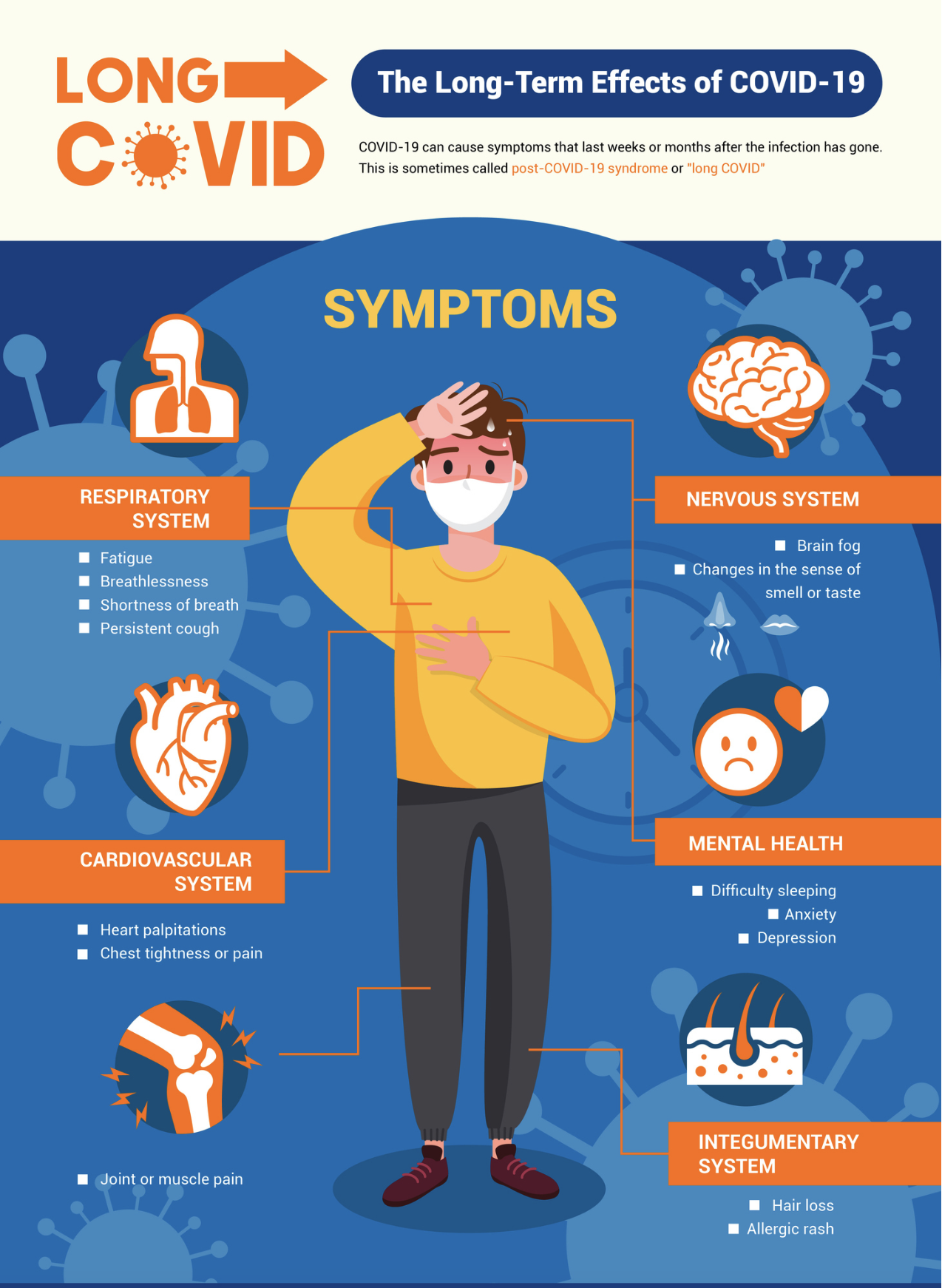
What might seem peculiar is that one COVID long hauler (as they are sometimes called) may not look anything like the next. The list of potential Long COVID symptoms is a lengthy one that may still be growing. Some of the most common ones will sound familiar, since they are the same symptoms often seen during the initial illness: fatigue, shortness of breath, fever, cough, difficulty thinking or concentrating (i.e., brain fog), and other problems with thinking, reasoning, or remembering.
But some long haulers report more unusual symptoms that seem very different from the illness that caused them. A colleague of mine has tinnitus (ringing in the ears). Another friend described an alcohol intolerance that set in after she had COVID last year, a symptom that’s yet to be well-investigated. Also, far from the breathing issues we first think of, those with COVID can experience menstrual pain and changes to the menstrual cycle, or persistent mental health issues, like depression, which persist for some COVID long haulers. Insomnia and digestive issues are yet other recognized symptoms.
Why the variety? Because Long COVID isn’t just one thing. According to the American Medical Association, there are three different categories of Long COVID.
COVID continues. The virus damaged your cells and they haven’t recovered, so the symptoms remain. Fatigue, shortness of breath, or loss of taste and smell — symptoms that lasted only a week or two for most COVID sufferers — continue months later, even after the virus is no longer on the attack.
New symptoms after COVID. New post-COVID symptoms can appear because a person’s immune and inflammatory systems aren’t working together properly. Inflammation is only supposed to happen when someone’s body gets damaged, and the immune system is only supposed to work against things that aren’t part of someone’s own body. For people in this category, either the inflammatory or the immune system — or both — are ramped up much more than they should be. This may account for some of the more unusual symptoms reported by COVID long haulers.
Effects of chronic hospitalization. These symptoms are not caused by the COVID infection itself, but by the long-term effects of being hospitalized and/or bedridden. Muscle weakness and post-traumatic stress disorders are examples.
The Good News
Omicron appears to cause fewer cases of Long COVID than its predecessor, Delta. (If you’ve already had Long COVID though, getting infected again is likely to trigger a recurrence — or to worsen the symptoms you already have.)
And as always, there are things you can do to reduce your risk:
Vaccination reduces your chances of getting Long COVID, so keep up on your vaccinations and boosters.
Early research also suggests that taking Paxlovid will reduce your Long COVID risk.
Information on Long COVID is expanding, and what we learn can only help us to respond better. You can learn more about the research being done, or even join a study yourself.
The best way to avoid Long COVID (or having symptoms recur or intensify) is to avoid getting COVID. I know it’s easier said than done, but for tips on how to reduce your risk, visit the "Stay Healthy" section on WhenToTest.org.